Depo-Provera is an injectable contraceptive that delivers a synthetic progestin intended to mimic the hormone progesterone.
In the United States, Depo-Provera and Depo SubQ Provera 104 are at the center of expanding pharmaceutical litigation focused on allegations that prolonged exposure may be linked to meningioma.
Many plaintiffs report that they were receiving Depo-Provera injections for years before learning they had a meningioma, often after headaches, vision changes, seizures, or other neurological symptoms prompted imaging.
The theory advanced in many complaints is that the use of Depo-Provera increases the risk of developing meningiomas, and that the drug’s progestin activity may contribute to tumor growth in susceptible patients.
These lawsuits typically frame the issue as a warning and patient-safety case rather than a dispute about whether the medication works as contraception.
As more cases have been filed, the federal judiciary centralized many of them into multidistrict litigation (MDL) to coordinate discovery and pretrial rulings across similar claims.
That centralized docket is designed to reduce duplicative proceedings while allowing each claimant to preserve an individual right to pursue damages based on personal medical history and outcomes.
Within that structure, the parties litigate what the science shows, what risks were known or reasonably knowable, and what the labeling communicated to prescribers and patients.
For many families, the lawsuits are also about accountability for the medical and financial disruption that can follow a meningioma diagnosis, treatment, and long-term monitoring.
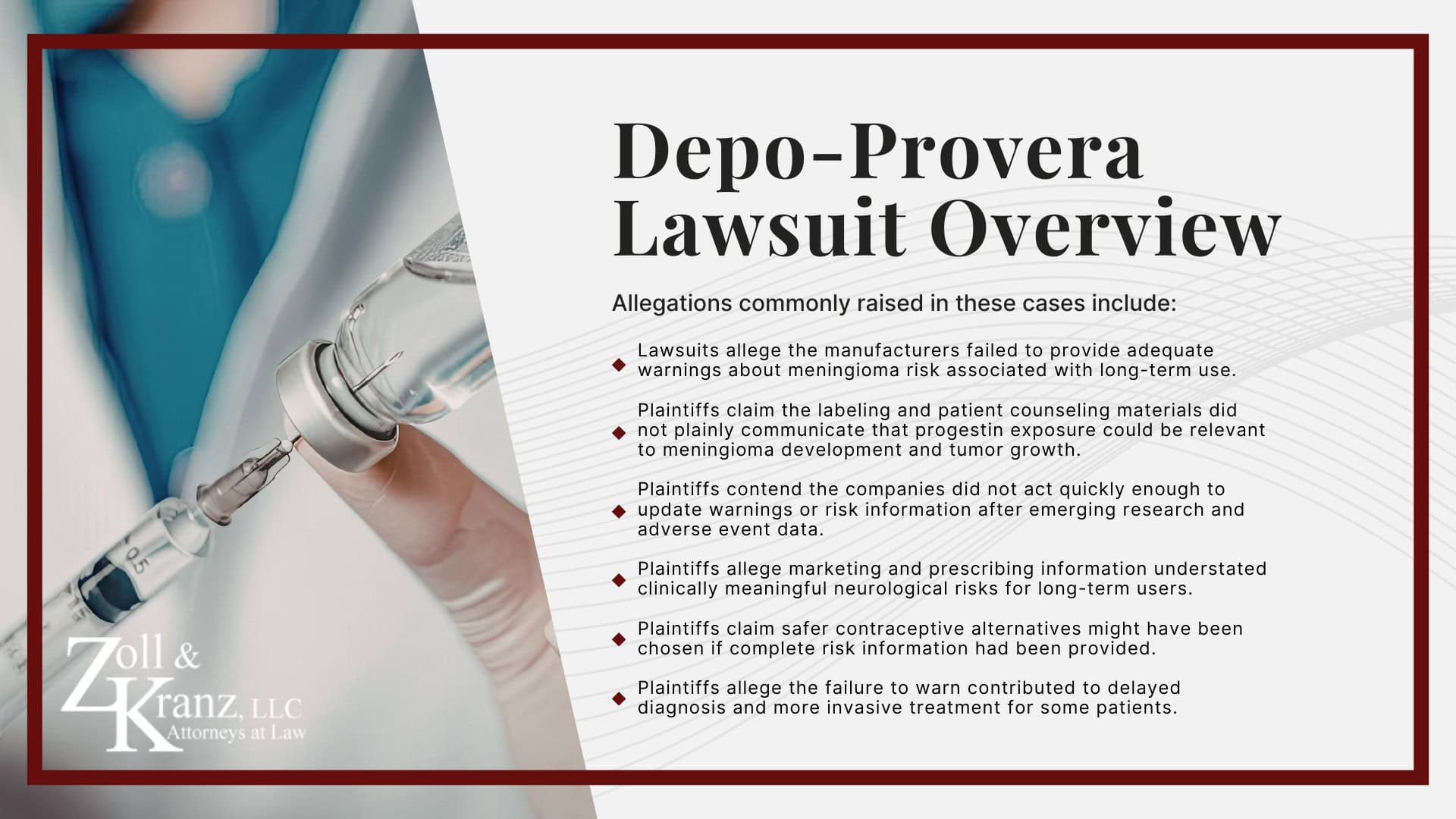
Allegations commonly raised in these cases include:
- Lawsuits allege the manufacturers failed to provide adequate warnings about meningioma risk associated with long-term use.
- Plaintiffs claim the labeling and patient counseling materials did not plainly communicate that progestin exposure could be relevant to meningioma development and tumor growth.
- Plaintiffs contend the companies did not act quickly enough to update warnings or risk information after emerging research and adverse event data.
- Plaintiffs allege marketing and prescribing information understated clinically meaningful neurological risks for long-term users.
- Plaintiffs claim safer contraceptive alternatives might have been chosen if complete risk information had been provided.
- Plaintiffs allege the failure to warn contributed to delayed diagnosis and more invasive treatment for some patients.
The goal of this legal action is to secure compensation tied to the injuries and losses alleged to flow from meningioma, including treatment costs, lost income, and long-term effects.
The litigation also aims to test whether manufacturers met their duties to communicate known or knowable risks to prescribers and patients.
Like many MDL proceedings, the outcome can turn on expert evidence about causation, the adequacy of warnings, and whether the claimed mechanism of harm is supported by medical research.
How is Depo-Provera Use Linked to Brain Tumors?
Depo-Provera is a form of birth control injections that delivers depot medroxyprogesterone acetate (DMPA), a long-acting synthetic progestin.
The litigation focus is on meningioma, a typically non-malignant tumor that arises from the meninges, the tissue layers that surround the brain and spinal cord.
In epidemiology and neurosurgical literature, meningiomas are commonly described as the most frequent primary intracranial tumors, and they account for roughly 30% to 40% of primary central nervous system tumors.
That “most common” label matters in a lawsuit context because a common tumor can still be a severe diagnosis for an individual patient.
The baseline incidence is often cited around 9.5 cases per 100,000 people per year in general population estimates, with incidence increasing substantially with age.
When meningiomas become symptomatic, the symptoms can include chronic or worsening headaches, vision changes, hearing changes, seizures, and memory problems, and the presentation often depends on where the tumor is located.
BMJ Study Links Depo-Provera Use to Brain Tumor Risk
The study most frequently cited in public reporting and legal filings is a large French national case control analysis published in The BMJ.
The authors reported that prolonged use of certain progestogens was associated with increased risk of intracranial meningioma, including for injectable medroxyprogesterone acetate, and a related BMJ Group summary highlighted a 5.6-fold increased risk with prolonged use of the medroxyprogesterone acetate injection, with no increased risk observed for less than one year of use in that analysis.
This finding is frequently described in plain language as “women using Depo-Provera for over a year are about 5 times more likely to develop meningioma than non-users,” although the exact comparator group and exposure definitions vary by study design.
Researchers Have Considered the Link for Decades
The idea that hormones could matter in meningioma biology did not start with the current lawsuits.
Researchers were studying hormone receptor activity in meningiomas decades ago, including work in the early 1980s examining estrogen and progesterone binding sites in these tumors.
That long-running biologic context supports the plausibility argument plaintiffs rely on: if many meningiomas are hormone-responsive, then long-term exposure to a potent progestin could, in some patients, contribute to the development or growth of a tumor.
Depo-Provera Label Update: Brain Tumor Risk Added in December 2025
In December 2025, the FDA-approved U.S. label for Depo-Provera was updated to add explicit meningioma warning language, including directions to discontinue Depo-Provera if meningioma is diagnosed and to monitor for signs and symptoms.
For litigation, this matters because lawsuits are not only about whether an association exists, but also about whether the risk information was communicated in a way that allowed informed prescribing and informed consent before patients committed to long-term use.
Settlement Projections for Depo-Provera Claims
Depo-Provera lawyers estimate that, if this litigation reaches a settlement phase, individual payouts could fall in a broad range from around $100,000 to over $1 million.
These figures are not guarantees of compensation, and they should not be read as a promise that any claimant will receive a particular amount.
They are estimates drawn from how other mass tort and product liability cases involving dangerous drugs and serious, documented injuries have sometimes resolved when liability and causation evidence supported global negotiations.
The value of any Depo-Provera claim can vary sharply based on tumor type and location, whether surgery or radiation was required, long-term neurological effects, and how clearly medical records support causation and damages.

Awards or settlements, if they occur, can also depend on litigation factors like the strength of expert testimony, admissibility rulings, and the timing and content of warnings at issue.
Some claims may be worth less than $100,000, while others may exceed $1 million, particularly where treatment was extensive and the patient has lasting impairment.
Any settlement range discussion should be treated as a general reference point only, because outcomes are case-specific and no lawyer can ethically predict a result for an individual without reviewing the facts.